Goals, Outcomes, Risks
Goals of Collaboration
 There can be multiple goals in a collaboration. In this image an integrated primary care and public health outreach service being delivered from a van. This example illustrates a number of potential collaboration goals.
There can be multiple goals in a collaboration. In this image an integrated primary care and public health outreach service being delivered from a van. This example illustrates a number of potential collaboration goals.
For example,
- Improving access to health services by removing barriers;
- Providing services to vulnerable populations;
- Addressing population needs and filling gaps, such as community mental health services;
- Providing client-centred care to target populations;
- Providing comprehensive health promotion and prevention services;
- Delivering effective harm reduction services, such as a needle exchange program.
 In this image, primary care and public health staff are working together with other community partners to plan stronger services to address women’s health in their northern community. Goals for the collaboration in this example can include:
In this image, primary care and public health staff are working together with other community partners to plan stronger services to address women’s health in their northern community. Goals for the collaboration in this example can include:
- Strengthening the collaborative partnership itself,
- Improving work processes such as increasing efficiencies or improving information sharing systems,
- Developing public policy and advocating for it.
Collaboration can also involve capacity building of the primary care and/or the public health workforce. Goals for such a collaboration can be:
- Increasing the uptake of evidence-based care,
- Creating healthier workplaces.
Impacts and Outcomes
Improved health of the population:
There are a number of perceived population health outcomes that have been reported by partners working in collaborations.
For example, collaborations have resulted in enhanced public policy and advocacy work, greater awareness by all partners of community problems, a shift to a population focus in programs, and improved population health status such as improved immunization rates, and reduced tobacco use.
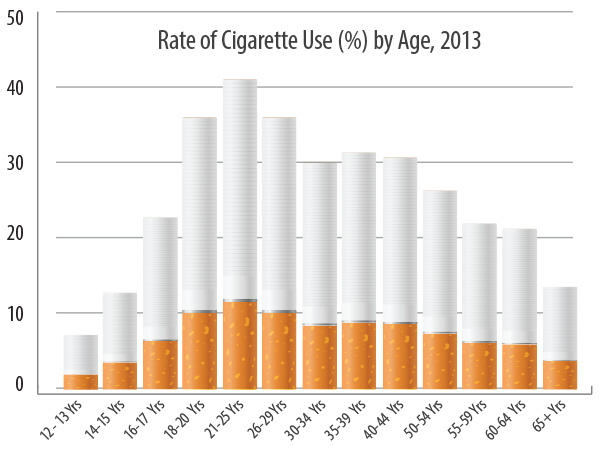
Graph for illustrative purposes only.
 Collaborations can result in improved health care effectiveness and efficiency, such as through improved quality of care and models of service delivery. Other outcomes include more continuity of care, enhanced sharing of information through integrated information systems, improved work processes evidenced by stronger networks of support, improved access to resources, and enhanced communication processes with partners.
Collaborations can result in improved health care effectiveness and efficiency, such as through improved quality of care and models of service delivery. Other outcomes include more continuity of care, enhanced sharing of information through integrated information systems, improved work processes evidenced by stronger networks of support, improved access to resources, and enhanced communication processes with partners.
Person-centred/person-directed care can also be achieved through collaborations where stronger relationships between clients and providers are developed. Trust can be developed between service providers and youth through a jointly run youth program.
Safer care is another potential collaboration outcome as community capacity is built for harm reduction services, or outbreak management is improved.
More timely care can be achieved as in the example of reduced wait times for immunizations. This resulted from the implementation of integrated information systems aimed to enhance primary care and public health scheduling and record keeping.
Other possible outcomes are related to more accessible and equitable programs and services. Examples are easier access to care through stronger referral systems and the development of new services through collaborations that increase reach. More equitable care can also be achieved as access is increased to marginalized populations.
Outcomes at the Organizational and Provider Level
 Outcomes have been realized in collaborations at the partner organization and the provider level. For example, improved relationships can result at the organizational level as well as between individual providers in the collaboration.
Outcomes have been realized in collaborations at the partner organization and the provider level. For example, improved relationships can result at the organizational level as well as between individual providers in the collaboration.
There can also be increased valuing and greater recognition of the partnership and individuals in it. Finally, staff can gain increased knowledge and skills in relation to their practice as well as gain a stronger understanding of each other’s roles and functions.
Finally there are potential positive economic outcomes resulting from primary care and public health collaboration. For example, there can be cost savings through resource allocation, reduced vaccine wastage, leverage information systems, reduced workload for partners, and resource development and sharing.
Listen to a public health manager describe their economic as well as other positive outcomes resulting from a collaboration with primary care practices in their region. The program manages vaccines and immunization records.
Drawbacks and Risks
- Collaboration can be one sided;
- Some benefit more than others;
- Difficult to impact public policy; difficult to measure impact (i.e., prevention);
- Diversion of resources from other services;
- Added workload for practitioners.
There are also a few potential risks or drawbacks of collaboration. For example, collaborations can benefit one partner more that the other. Diversion of human resources from usual activities to developing and maintaining the collaboration has also been reported as a drawback. Finally, some collaborations have resulted in added workload for partners to engage in collaborations.
Collaboration partners generally agree that the benefits of collaboration outweigh the drawbacks. However, it is important to evaluate the perceptions of individuals who are working in the collaboration to identify any potential drawbacks and risks that may exist as part of a quality improvement process. ![]() The Evaluation and Research Module provides resources such as links to the Partnership Self-Assessment Tool which measures perceived benefits versus drawbacks.
The Evaluation and Research Module provides resources such as links to the Partnership Self-Assessment Tool which measures perceived benefits versus drawbacks.
The most effective way to address potential drawbacks and risks is to consider using the framework and related materials as a resource.
